Abstract

Introduction:
Multiple myeloma diagnosis is associated with a 10-15% absolute risk of venous thromboembolism (VTE) due to disease-related (i.e., vascular inflammation, hyperviscosity) and treatment-related risk factors (i.e., immunomodulatory drugs [IMiDs], high-dose dexamethasone). This has led to ongoing clinical trials to determine the best thromboprophylaxis strategy. In contrast, the risk of major bleeding following incident VTE events in patients with MM is not well described. We conducted a real-world analysis of bleeding complications in MM following anticoagulation treatment for VTE.
Methods:
The IBM MarketScan Commercial Claims Database was used to identify adults with MM diagnosis and an incident VTE event between 2011 and 2019. MM and VTE were defined as 1 inpatient or 2 outpatient claims based on International Classification of Diseases (ICD) 9th and 10 th Revision codes, and at least 1 prescription for anticoagulation within 31 days of first VTE claim. IMiD-related VTE was defined in subjects with an IMiD prescription prior to the VTE event. Major bleeding was defined as bleeding requiring hospitalization using inpatient ICD codes as previously validated (Cunningham algorithm). Patients were followed from index VTE and initiation of anticoagulation to first major bleeding event, disenrollment (due to death or other reasons) or December 31, 2019. Descriptive statistics were used to calculate the rate of major bleeding. Cox regression was used to determine risk factors associated with major bleeding.
Results:
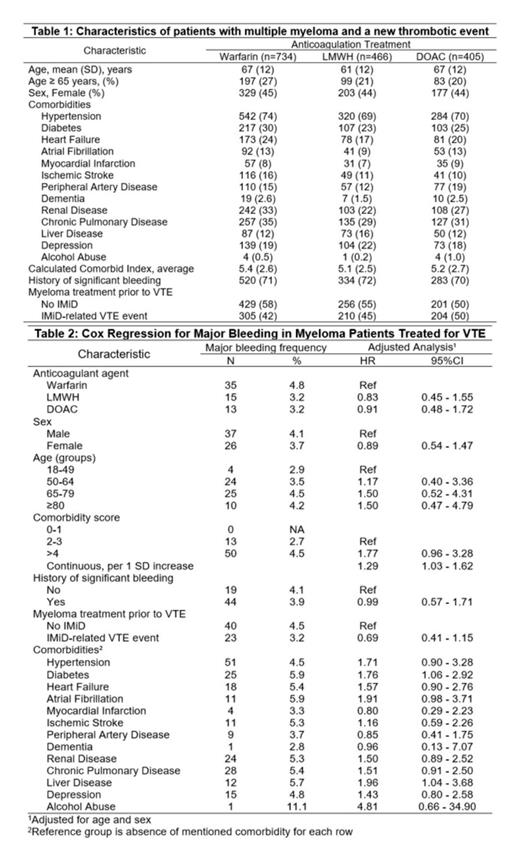
Our population included 1,605 patients with a diagnosis of multiple myeloma and an incident VTE event requiring treatment. Anticoagulant agent of choice was warfarin in 45.7% (734), low-molecular weight heparin (LMWH) in 29% (466), and direct oral anticoagulants (DOAC) in 25.3% (405). There were no significant differences in age/sex distribution, comorbidity burden, history of significant bleeding, or use of IMiD across the different types of anticoagulation (Table 1). Hospitalized bleeding occurred in 63 (3.9%) patients during an average follow-up of 1.6 years, yielding an overall incidence rate of major bleeding in multiple myeloma patients starting anticoagulation for a new VTE event of 24.1 per 1,000 person-years. Adjusting for age and sex, risk factors significantly associated with risk of major bleeding included Charlson comorbidy index [CCI] (per standard deviation [SD] increment, HR 1.29, 95%CI 1.03 - 1.62), diabetes (HR 1.71, 95%CI 1.06 - 2.92), and liver disease (HR 1.96, 95%CI 1.04 - 3.68). The use of IMiDs was not associated with increased risk of major bleeding (Table 2). The cumulative incidence of major bleeding by VTE anticoagulation strategy in multiple myeloma was 4.8% in warfarin group and 3.2% in the LMWH and DOAC groups, though the difference was not statistically significant after adjusting for age and sex. The estimated incidence rate of bleeding was 25.7, 20.1, and 25.2 per 1,000 person-years for patients treated with warfarin, LMWH, and DOACs, respectively. In an adjusted model for age, sex, CCI, diabetes and liver disease, patients treated with LMWH and DOACs had HR for major bleeding of 0.91 and 0.82, respectively, compared to anticoagulation with warfarin, though this was not statistically significant.
Discussion:
In a real-world analysis of commercial claims data, the rate of major bleeding in patients with multiple myeloma receiving anticoagulation for VTE appears to be comparable to those reported in other subsets of cancer associated VTE. Surprisingly, almost half of identified patients were treated with warfarin, a non-preferred option in this setting. The point estimate of major bleeding was lower in patients treated with LMWH or DOACs compared to warfarin, though the association was not statistically significant and larger studies are needed. Higher CCI, diabetes and liver disease were clinical factors associated with higher risk of major bleeding and may be included in risk assessment models to help clinicians assess individual bleeding risk in patients with multiple myeloma treated for VTE.
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract